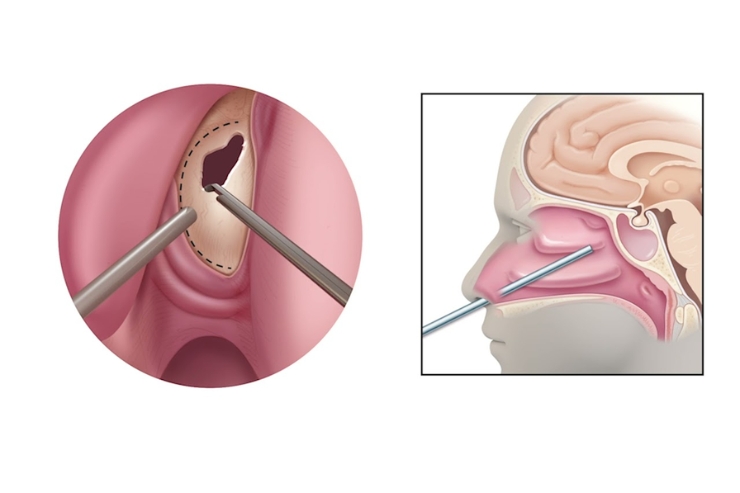
Endoscopic or open resection of anterior skull base and sinonasal tumors involves surgically removing malignant or benign growths originating from the nasal cavity, paranasal sinuses (ethmoid, frontal, maxillary), or the anterior cranial base. In endoscopic approaches, specialized nasal endoscopes and angled instruments are introduced through the nostrils to excise tumors with minimal external incisions. Open approaches (e.g., lateral rhinotomy, craniofacial resection) access extensive or externally extending lesions via carefully planned scalp and facial incisions, allowing direct visualization of the tumor and adjacent critical structures such as the dura, orbit, and neurovascular bundles. Dr. Hitesh R. Singhavi tailors each technique to tumor size, location, and invasion pattern.
Preoperatively, Dr. Singhavi orders high-resolution CT and MRI with contrast to map tumor boundaries, bone erosion, and dural involvement. A multidisciplinary skull-base team—including neurosurgeons, otolaryngologists, and radiologists—reviews imaging in a tumor board. For tumors confined medially without lateral orbital invasion, he favors an endoscopic endonasal resection to preserve facial aesthetics and reduce morbidity. In cases with extensive lateral disease, dural breach, or intracranial involvement, a combined open craniofacial resection is planned. Intraoperative neuronavigation and endoscopic fluorescence guidance (e.g., 5-ALA) help delineate tumor margins. Frozen‐section pathology confirms clear margins before reconstruction. When defects involve the dura or skull base, Dr. Singhavi coordinates microvascular free-flap reconstruction (e.g., radial forearm or anterolateral thigh) and multilayer duraplasty to prevent cerebrospinal fluid leaks. Postoperative care includes head elevation, careful fluid management, and prophylactic antibiotics.
Under Dr. Singhavi’s meticulous execution, patients benefit from complete tumor clearance with preservation of critical functions—smell, vision, and brain protection—while minimizing cosmetic deformity. Endoscopic resections deliver reduced blood loss, shorter anesthesia time, and faster recovery, with many patients discharged within 2–3 days. When open approaches are necessary, modern incision planning and free-flap reconstruction restore seamless skull base integrity and facial contour, reducing long-term complications such as enophthalmos and cranial nerve deficits. Rigorous margin control and reconstructive excellence lower recurrence rates, prevent cerebrospinal fluid leaks, and enable rapid rehabilitation—ensuring patients can resume normal breathing, olfaction, and daily activities with confidence.