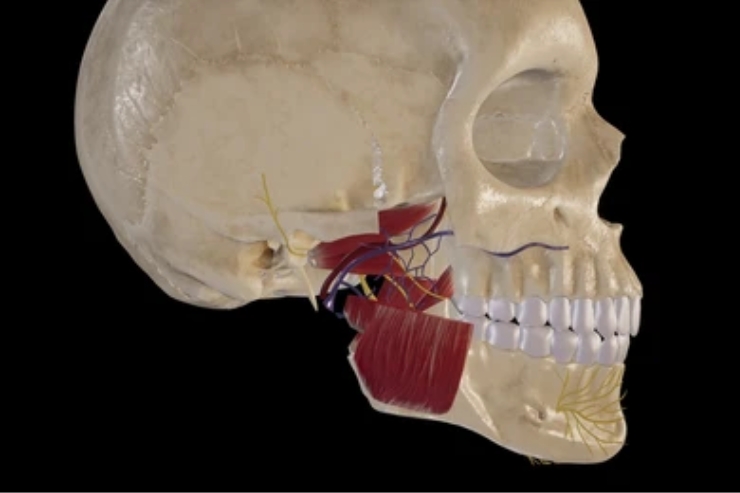
Infratemporal fossa tumors—arising from deep masticator spaces, pterygoid muscles, or cranial base foramina—pose significant surgical challenges due to limited access and proximity to critical structures (cranial nerves III–VI, internal carotid artery). Resection typically requires extended approaches (e.g., Fisch temporal or preauricular infratemporal fossa approach) to safely expose and remove the lesion.
Dr. Singhavi utilizes contrast CT angiography and MRI to visualize tumor relationships to the skull base, vessels, and nerves. A preoperative embolization protocol—performed by interventional radiology—is considered for highly vascular lesions to minimize intraoperative bleeding. Under general anesthesia, he selects the optimal approach: a preauricular or transzygomatic corridor for lateral tumors; or a transmaxillary route for medially situated lesions. Osteotomies of the zygomatic arch and coronoid process enhance exposure. Intraoperative neuro-monitoring tracks cranial nerve function continuously. Once the tumor is removed en bloc, he reconstructs bony defects with patient-specific titanium plates and soft-tissue flaps (radial forearm or pectoralis major) to obliterate dead space and protect neurovascular structures. Postoperative protocols include head-of-bed elevation, cranial nerve assessments, and dedicated physiotherapy for mandibular function.
Through Dr. Singhavi’s advanced skull-base expertise, patients receive complete resection of challenging infratemporal fossa tumors with minimized neurologic morbidity. Preoperative planning and selective embolization reduce operative time and transfusion needs. The tailored approach preserves facial nerve and masticatory muscle function, maintaining jaw mobility and sensation. Customized reconstruction secures mechanical stability, preventing cerebrospinal fluid leaks and contour deformities. Patients benefit from shorter ICU stays, early enteral feeding, and a streamlined recovery pathway—ensuring rapid return to baseline activities and sustained cranial integrity.